finger guide

Finger splints offer crucial support for various hand conditions‚ aiding recovery and function. They’re utilized post-injury‚ during rehabilitation‚ or to manage chronic ailments.
What is a Finger Splint?
A finger splint is a medical device used to immobilize and support a finger or fingers. These supports can range from simple‚ over-the-counter options to custom-fabricated devices created by a therapist or orthotist. They are typically constructed from materials like metal‚ plastic‚ or thermoplastic‚ and are designed to restrict movement‚ promoting healing and preventing further injury.
Splints come in various forms – from rigid structures offering complete immobilization to more flexible designs allowing limited motion. Their primary function is to maintain a specific finger position‚ correct deformities‚ or protect injured tissues. They are a non-invasive treatment option‚ often employed as a first line of defense in managing a wide array of hand and finger conditions.
Why Use a Finger Splint?
Finger splints are employed for a multitude of reasons‚ primarily to protect and support injured or weakened fingers. They’re crucial after fractures or dislocations‚ ensuring proper alignment during the healing process. For tendon injuries‚ splints minimize strain and facilitate recovery by restricting potentially damaging movements.
Beyond acute injuries‚ splints effectively manage chronic conditions like arthritis‚ reducing pain and preventing joint deformation. Neurological conditions‚ such as those resulting from brain injury or cerebral palsy‚ benefit from splints that maintain functional hand positions and combat spasticity. Ultimately‚ splints aim to improve hand function‚ reduce discomfort‚ and enhance overall quality of life.
Types of Finger Splints
Finger splints vary in design – static‚ dynamic‚ and serial – each offering unique support levels and movement capabilities tailored to specific conditions and recovery phases.
Static Splints
Static splints are designed to immobilize a finger joint or joints in a specific position. They provide support and prevent movement‚ allowing tissues to heal without disruption. These splints are typically made from materials like thermoplastic or metal and are molded to the individual’s finger.
Their primary function is to maintain alignment and prevent contractures – the shortening or tightening of muscles‚ tendons‚ or ligaments. Static splints are often used after fractures‚ dislocations‚ or surgeries where complete immobilization is crucial for proper healing. They don’t actively assist with movement; instead‚ they hold the finger in a predetermined‚ beneficial position. Adjustments are minimal once applied‚ focusing on maintaining the established alignment throughout the healing process.
Dynamic Splints
Dynamic splints differ from static splints by actively assisting with movement and promoting joint mobilization. They utilize tension systems – often rubber bands or springs – to gently stretch or reposition the finger towards a desired range of motion. These splints are particularly useful when a patient has limited ability to move a joint independently due to weakness‚ pain‚ or stiffness.
Unlike static splints that simply hold a position‚ dynamic splints provide a continuous‚ low-load force that encourages gradual improvement in joint flexibility and function. They are frequently employed after tendon repairs‚ neurological conditions‚ or to address contractures where regaining movement is a primary goal. The tension can be adjusted to accommodate the patient’s progress and tolerance‚ making them a versatile rehabilitation tool.
Serial Splints
Serial splints represent a unique approach to regaining finger motion‚ particularly when dealing with significant contractures – a permanent shortening of muscles or tendons. This technique involves applying a static splint to gradually increase the range of motion over time. The splint is worn for a specific period‚ typically several days‚ positioning the finger slightly beyond its current comfortable range.
After this period‚ the splint is removed‚ and the finger is passively moved to the new‚ slightly improved position. A new splint is then applied‚ holding this new position. This process is repeated incrementally‚ “serially” advancing the finger’s range of motion. It’s a slow but effective method‚ minimizing discomfort and maximizing gains in flexibility‚ often used when other methods have limited success.

Conditions Treated with Finger Splints
Finger splints effectively address diverse conditions‚ including arthritis‚ tendon injuries‚ fractures‚ neurological impairments like cerebral palsy‚ and post-surgical recovery needs.
Arthritis and Finger Splints
Arthritis‚ a common cause of finger pain and stiffness‚ significantly benefits from finger splint utilization. Splints help maintain proper joint alignment‚ reducing stress and discomfort. They can minimize inflammation and prevent further joint damage‚ particularly in rheumatoid or osteoarthritis cases.
Splints support weakened finger joints‚ enabling continued hand function during daily activities. They can be especially helpful for individuals experiencing morning stiffness or pain that worsens with use. Different splint types cater to varying arthritis stages and symptoms‚ from simple support splints to more dynamic options promoting joint movement. Consistent use‚ as directed by a healthcare professional‚ is key to maximizing benefits and improving quality of life for those managing arthritic conditions.
Tendon Injuries and Splinting
Tendon injuries in the fingers‚ such as mallet finger or boutonniere deformity‚ frequently require splinting for effective healing. Splints immobilize the affected joint‚ protecting the injured tendon from further strain and allowing it to mend properly. The specific type of splint and duration of wear depend on the injury’s severity and location.
Splinting prevents unwanted movement that could disrupt the healing process‚ ensuring optimal tendon alignment. Dynamic splints‚ in particular‚ can gently encourage tendon gliding and restore range of motion as healing progresses. Following a healthcare provider’s instructions regarding splint wear and rehabilitation exercises is crucial for a successful recovery and regaining full finger function. Ignoring these guidelines can lead to chronic pain or limited dexterity.
Fractures and Dislocations
Finger fractures and dislocations often necessitate immediate splinting to stabilize the injury and minimize pain. A splint provides essential support‚ preventing further displacement of the bone fragments or joint surfaces. This immobilization is critical for proper healing and reduces the risk of complications like malunion or chronic instability;
The type of splint utilized will vary based on the fracture’s location and severity‚ or the nature of the dislocation. Often‚ buddy taping – securing the injured finger to an adjacent‚ uninjured one – serves as an initial stabilization method. More complex injuries may require a rigid splint extending beyond the affected joint. Consistent monitoring by a healthcare professional is vital to ensure appropriate healing and guide the transition to rehabilitation exercises.
Neurological Conditions & Splints (Brain Injury‚ Cerebral Palsy)
Neurological conditions like brain injury or cerebral palsy can significantly impact hand function‚ often leading to spasticity‚ weakness‚ or impaired coordination. Finger splints play a crucial role in managing these challenges‚ aiming to improve hand positioning‚ prevent contractures‚ and enhance functional abilities.
For individuals with spasticity‚ dynamic splints can gently stretch and realign the fingers‚ reducing muscle tightness. Splints can also provide support for weakened hands‚ enabling participation in daily activities. In cases of cerebral palsy‚ early intervention with splinting can help optimize motor development. The selection and application of splints require a thorough assessment by an occupational therapist to tailor the intervention to the individual’s specific needs and goals‚ promoting independence and quality of life.
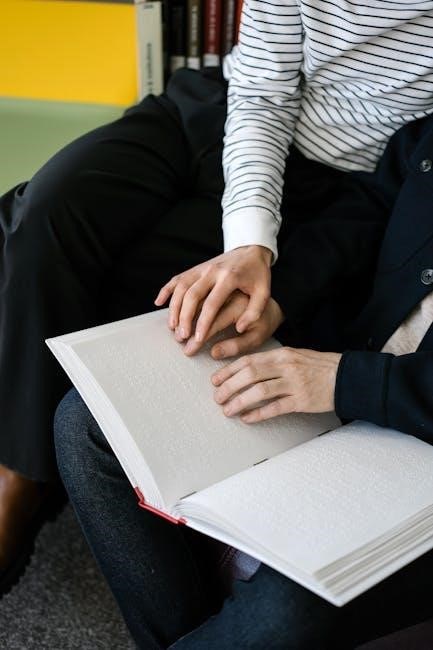
Applying a Finger Splint: A Step-by-Step Guide
Proper application involves finding the correct finger‚ securing a suitable splint‚ and wrapping it firmly for support and stability during the healing process.
Preparing the Finger
Before applying any finger splint‚ meticulous preparation is essential for optimal results and patient comfort. Begin by gently cleaning the affected finger and surrounding skin with mild soap and water‚ ensuring complete dryness to prevent skin irritation under the splint.
Assess the finger for any open wounds‚ abrasions‚ or signs of infection; if present‚ address these concerns with a healthcare professional before proceeding. Carefully examine the range of motion and note any limitations or pain points.
Position the finger in the desired therapeutic position – often a slight bend – as dictated by the specific condition and treatment plan. Padding may be applied to bony prominences or sensitive areas to minimize pressure and enhance comfort during splint wear.
Attaching Finger Loops
Securely attaching finger loops is a critical step in ensuring the splint’s effectiveness and proper alignment. Most finger splints feature openings designed to accommodate these loops‚ which provide a stable connection point for securing the splint to the digit.
Carefully thread the finger loops through these openings‚ ensuring they are positioned comfortably around the base of the finger and the proximal interphalangeal joint. Avoid overtightening the loops initially‚ allowing for some adjustability during the splinting process.
Double-check that the loops are evenly distributed and not causing any pressure points or constriction. Proper loop placement is vital for maintaining the correct finger position and preventing slippage of the splint.
Positioning the Splint
Correct splint positioning is paramount for achieving the desired therapeutic outcome. Once the finger loops are attached‚ gently slide the hand into the splint‚ ensuring the palmar bar aligns comfortably within the palm’s natural arch. This bar provides essential support and prevents unwanted flexion or extension of the fingers.
Verify that the finger being splinted is positioned in the prescribed angle or alignment‚ as determined by a healthcare professional. The splint should not restrict circulation or cause undue pressure on any part of the hand or fingers.
Carefully assess the overall fit‚ ensuring the splint conforms to the hand’s contours without creating any gaps or discomfort.
Securing the Splint with Rubber Bands
Securing the splint effectively is crucial for maintaining the correct finger position. Utilize rubber bands to connect the loops attached to the splint‚ creating gentle but firm tension. Begin with the loop closest to the base of the finger and progress towards the fingertip‚ applying even pressure with each band.
Avoid over-tightening the rubber bands‚ as this can compromise circulation and cause discomfort. Regularly check the color and temperature of the fingertip to ensure adequate blood flow.
The rubber bands should hold the splint securely in place without restricting movement beyond the intended limitations. Adjust band placement as needed to achieve optimal support and comfort.

Splint Wearing Schedules & Considerations
Splint wear duration varies based on the condition; consistent use is key for optimal results. Monitor skin closely‚ adjusting fit to prevent irritation or discomfort.
Duration of Wear
Determining the appropriate duration for wearing a finger splint is highly individualized and depends significantly on the underlying condition being addressed. For acute injuries like fractures or dislocations‚ splints are often worn for several weeks to provide immobilization and facilitate healing.
In cases of arthritis or tendon injuries‚ the wearing schedule might be more intermittent‚ focusing on periods of activity or when symptoms are exacerbated. Some individuals may benefit from wearing a splint only during nighttime to maintain proper joint alignment while sleeping.
Following a healthcare professional’s guidance is paramount‚ as they will tailor the duration to your specific needs and monitor your progress. Prematurely discontinuing splint use can hinder recovery‚ while prolonged use without reassessment may lead to muscle weakness or stiffness.
Monitoring for Skin Irritation
Consistent skin checks are vital when wearing a finger splint to prevent complications. Prolonged contact between the splint material and skin can cause irritation‚ redness‚ or even breakdown. Regularly inspect the skin around and under the splint for any signs of pressure sores‚ blisters‚ or rashes.
Pay close attention to areas where the splint edges rub against the skin. If irritation develops‚ consult your healthcare provider. They may recommend adjusting the splint‚ using padding‚ or modifying the wearing schedule.
Maintaining good hygiene is also crucial; keep the skin clean and dry. Report any persistent discomfort or skin changes immediately to avoid potential infections or further complications. Early detection and intervention are key to ensuring comfortable and effective splint use.
Adjusting the Splint
Proper splint fit is essential for optimal effectiveness and comfort. If the splint feels too tight‚ restricting circulation‚ or too loose‚ providing insufficient support‚ adjustments are necessary. Begin by loosening the securing straps or rubber bands slightly. Re-apply‚ ensuring a snug but not constricting fit.
Observe for any signs of compromised circulation‚ such as numbness‚ tingling‚ or discoloration of the fingertip. If these occur‚ immediately loosen the splint further. Conversely‚ if the splint shifts excessively during use‚ tighten it cautiously.
Consult your healthcare professional for guidance on significant adjustments or if you are unsure about making changes yourself. They can ensure the splint continues to provide the appropriate level of support without causing harm.
Caring for Your Finger Splint
Regular cleaning with mild soap and water maintains hygiene. Avoid harsh chemicals. Store the splint in a cool‚ dry place when not in use for longevity.
Cleaning Instructions
Maintaining cleanliness is paramount for preventing skin irritation and infection while using a finger splint. Gently wash the splint regularly – ideally daily‚ or as needed – using lukewarm water and a mild‚ pH-neutral soap. Avoid abrasive cleaners‚ solvents‚ or strong detergents‚ as these can damage the splint material or leave irritating residues.
Use a soft cloth or brush to remove any dirt or debris. Rinse thoroughly to eliminate all soap residue. Pat the splint dry with a clean towel; avoid using direct heat sources like hairdryers‚ as this could warp or distort the shape. Ensure the splint is completely dry before reapplication to prevent moisture buildup and potential skin issues. Inspect the splint for any cracks or damage during cleaning.
Storage Guidelines
Proper storage extends the life of your finger splint and maintains its hygiene. When not in use‚ store the splint in a clean‚ dry‚ and cool environment‚ away from direct sunlight and extreme temperatures. A breathable storage bag or container is ideal‚ preventing dust accumulation while allowing air circulation.
Avoid storing the splint in humid locations like bathrooms‚ as moisture can promote bacterial growth. Keep it separate from other items that could cause scratches or damage. Regularly inspect the storage area for pests. If the splint is disassembled for cleaning or adjustment‚ store all components together to prevent loss. Following these guidelines ensures your splint remains in optimal condition for continued support and recovery.

Advanced Splinting Techniques
Custom splints‚ tailored to individual needs‚ and combining splints with assistive devices maximize function and support for complex hand injuries or conditions.
Custom-Made Splints
Custom-made finger splints represent a significant advancement in hand therapy‚ offering a highly personalized approach to treatment. Unlike prefabricated options‚ these splints are meticulously crafted based on precise measurements and a thorough understanding of the patient’s specific anatomy and condition. This level of customization ensures an optimal fit‚ maximizing comfort and therapeutic effectiveness.
The process typically involves creating a mold of the finger or hand‚ which is then used to fabricate a splint from materials like thermoplastic or acrylic. This allows for intricate designs that address unique challenges‚ such as correcting deformities‚ providing targeted support‚ or accommodating sensitive skin. Custom splints are particularly beneficial for individuals with complex injuries‚ chronic conditions‚ or those requiring a precise level of immobilization or mobilization.
They are often recommended when standard splints fail to provide adequate support or cause discomfort. A qualified occupational therapist or hand specialist will assess the patient’s needs and oversee the entire process‚ from initial evaluation to final fitting and adjustments.
Splinting with Assistive Devices
Integrating assistive devices with finger splints expands treatment possibilities‚ particularly for individuals facing neurological challenges like brain injury‚ cerebral palsy‚ or Parkinson’s disease. These combinations aim to enhance functional abilities and promote independence in daily living.
For example‚ splints can be paired with elastic assistance to facilitate finger extension or flexion‚ aiding individuals with limited range of motion. Similarly‚ incorporating specialized grips or handles onto splints can improve grasping and manipulation skills. Devices addressing tremors can also be combined‚ offering stability during tasks.
The selection of appropriate assistive devices depends on the specific functional limitations and goals of the patient. Occupational therapists play a crucial role in assessing needs‚ recommending suitable devices‚ and customizing the splint-assistive device combination for optimal effectiveness. Careful monitoring and adjustments are essential to ensure comfort and maximize therapeutic benefits.

Resources and Further Information
For comprehensive information on finger splints and hand therapy‚ several resources are readily available. The American Society of Hand Therapists (ASHT) provides a directory of certified hand therapists and educational materials at asht.org. Numerous online platforms offer detailed guides‚ videos demonstrating application techniques‚ and patient testimonials.
Consulting with a qualified occupational therapist is paramount for personalized guidance. They can assess your specific condition‚ recommend the most appropriate splint type‚ and develop a tailored treatment plan. Local hospitals and rehabilitation centers often host workshops and support groups for individuals undergoing hand therapy.
Remember to prioritize reliable sources and discuss any concerns with your healthcare provider. Proper splint usage and adherence to recommended exercises are crucial for optimal recovery and long-term hand function.